ICU Insulin Infusion Calculator
Author: John Paul Feliciano
In Collaboration With: My sister, an RN at RUHS
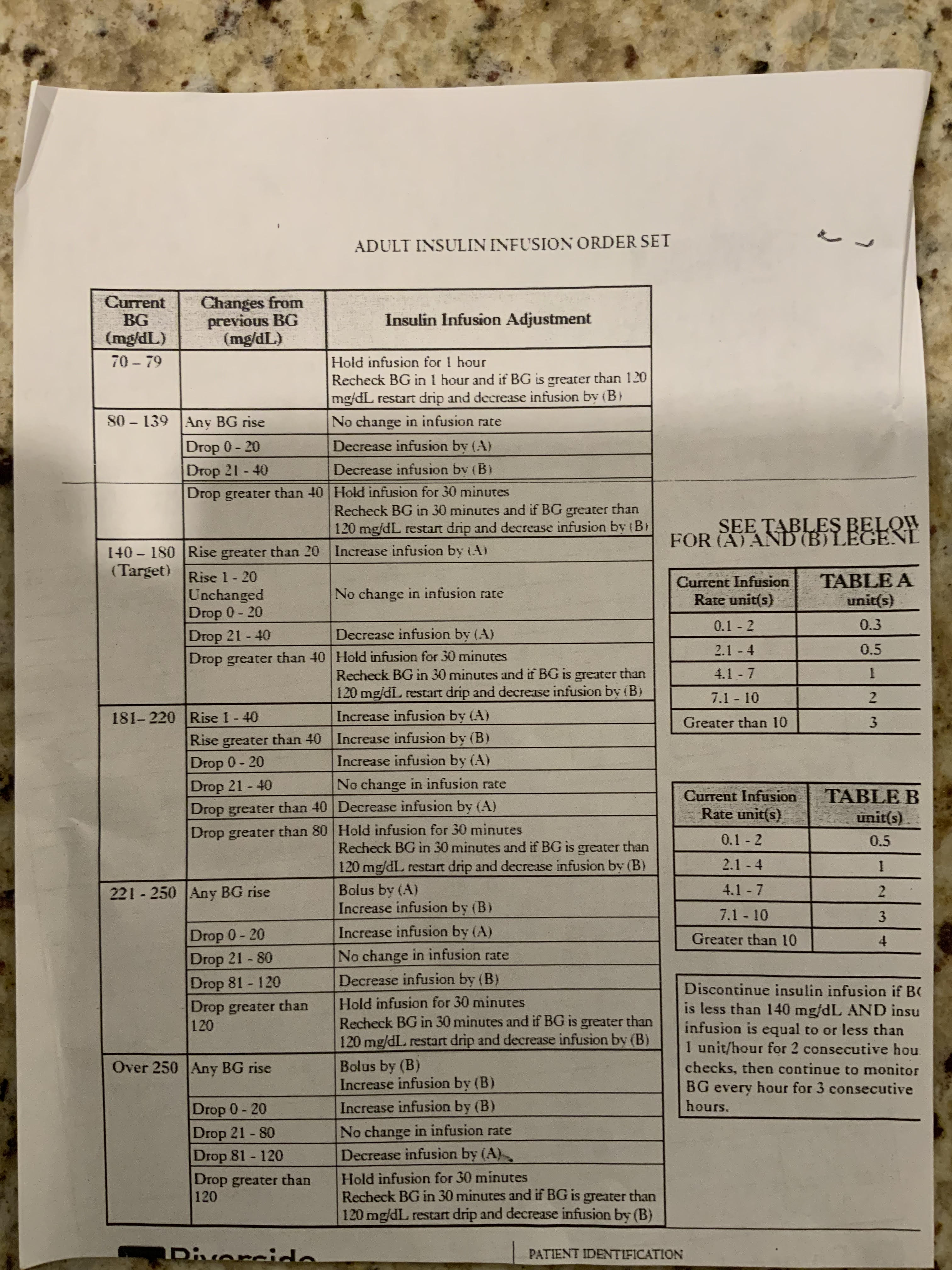
Digitizing the Physical Table
My sister works in the ICU at Riverside University Health System (RUHS), where she relies on a paper-based reference table to quickly adjust insulin drip rates for patients with varying blood sugar levels. Below is the photograph of that table:
Project Goal
This project transforms the paper reference into an interactive, web-based tool, significantly cutting down on calculation time and potential errors. By automating the drip-adjustment logic, ICU nurses can quickly get recommended actions—like “hold for 30 minutes” or “increase infusion rate by 0.5 units”—based on real-time blood glucose entries.
Key Features
- Automated Calculations: Enter current BG, previous BG, and infusion rate, and the tool applies the branching logic to give an immediate recommendation.
- Clarity and Consistency: Standardizes the protocol, reducing variation in how nurses interpret the table.
- Lightweight Flask App: Easy to deploy and maintain on local hospital intranets or via a simple hosting service.
- Updatable Rules: The infusion adjustment logic is modular, so any hospital policy changes can be quickly integrated.
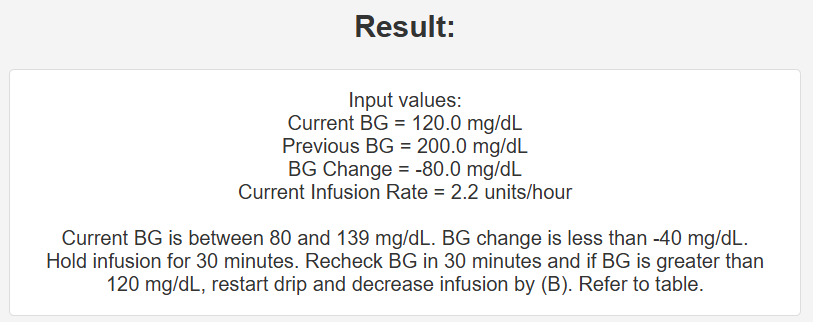
App Screenshots
Below are a couple of screenshots illustrating the user interface:
Form for BG & Infusion Inputs

Real-Time Recommendations
Tech Stack
- Backend: Flask (Python), with carefully structured conditional logic
- Frontend: HTML/Jinja templates; minimal custom CSS or Bootstrap
- Deployment: Hosted via PythonAnywhere (see link below)
- Local/Dev Usage: Run
python app.pyin a virtual environment for quick local testing
Development Highlights
- Paper-to-Code Mapping: Every row in the table was carefully translated into Python conditions and computations, ensuring all edge cases (e.g., big drops in BG) were covered.
- Real-World Testing: My sister tested in a simulated ICU environment, providing feedback on clarity, usability, and correctness of the recommendation text.
- Incremental Improvements: The instructions (e.g. "Hold infusion 30min") were refined multiple times to match real-world nurse workflows.
Challenges & Solutions
- Edge-Case Handling: Some rules overlapped or had intricate numeric thresholds. Solution: thorough unit testing of each possible BG range and infusion change scenario.
- Keeping It Nurse-Friendly: Medical staff prefer explicit instructions without unnecessary jargon. We kept outputs simple.
- Potential EHR Integration: While not yet implemented, the design anticipates an API approach for future auto-fetching of BG values from a patient’s EHR.
Lessons Learned
- Direct Nurse Involvement: The best feedback loop involves actual users (in this case, an ICU nurse) from day one of development.
- Lightweight Architecture: A simple Flask-based approach is sufficient for many clinical tools, especially internal hospital use.
- Documentation of Rule Changes: Keeping each threshold in a well-organized dataset (or JSON) can make policy updates straightforward.
Future Directions
- Data Tracking: Log each recommended change, building a patient-specific BG profile over time.
- EHR Integration: Automatic input from hospital systems to reduce manual typing and potential mis-entries.
- Expanded Medical Calculations: Incorporating additional ICU dosing protocols (e.g., sedation, vasopressors) for a broader critical-care tool.
Interested in More?
Live Demo: You can try the calculator here: ICU Insulin Infusion Calculator (Hosted on PythonAnywhere) .
Source Code: ICU Insulin Infusion Calculator